Artificial platelets reduce clotting time and blood loss
 Researchers at the Georgia Institute of Technology (Georgia Tech) have devised a new technology that could help the blood to clot faster, potentially reducing blood loss in wounded people. They developed artificial platelets – an artificial counterpart to components of blood that help with wound clotting or sealing. This biomaterial is made from hydrogel and laced with regulatory chemicals.
Researchers at the Georgia Institute of Technology (Georgia Tech) have devised a new technology that could help the blood to clot faster, potentially reducing blood loss in wounded people. They developed artificial platelets – an artificial counterpart to components of blood that help with wound clotting or sealing. This biomaterial is made from hydrogel and laced with regulatory chemicals.
The artificial platelets can be freeze-dried and could be put in an injector device the size of a smartphone. Soldiers wounded on the battlefield could use this device to help control bleeding and stabilize the injury while waiting for clinical treatment.
The first blood clot begins forming right after an injury. It is believed that this initial response may control subsequent healing process. In studies conducted on animals, the synthetic platelets reduced clotting time by 30 percent and blood loss by as much as 40 percent.
“The idea is to have on the battlefield technologies that would deliver a biomaterial capable of finding where the bleeding is happening and augmenting the body’s own clotting processes. Simultaneously, the material would help instruct the biochemistry and biophysics of the clot structure that would govern subsequent healing”, said Dr Thomas Barker, an associate professor in the department of biomedical engineering at Georgia Tech.
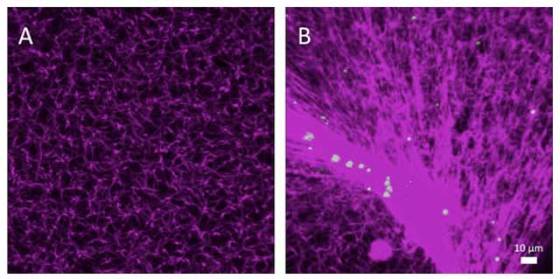
When injected into the body, the synthetic platelets circulate in the bloodstream until activated by proteins that activate natural blood clotting. Protein fibrinogen is the precursor for fibrin, the polymer that provides the basic structure for natural blood clots. When tissue damage results in bleeding, protein called thrombin sends signals which initiate conversion of fibrinogen into fibrin. Fibrin molecules then combine to form long fibrin threads that catch platelets, building up a mass that form the blood clot. The researchers use the same trigger to activate the artificial platelets. Activated platelets change shape and convert to a thin film that helps in wound sealing.
The molecule responsible for specific recognition is an antibody modified by researchers. They used bacteria growing on plate as a tool for evolving antibodies. These antibodies can be bound to hydrogels and has high affinity for fibrin and low affinity for fibrinogen. The antibody changes the shape of hydrogel when it encounters activated fibrin.
“We knew the molecule that we wanted and we knew the domains that were critical for recognition. The primary design concept was the ability to recognize an active, forming clot from the soluble, inactive precursor”, said Barker.
Georgia Tech research team is also developing a polymer with an attached natural peptide which regulates repair process that produces scars. The polymer could be used to prevent the formation of scars and fibrosis.
The artificial platelets have so far been tested on rats, hence much more research needs to be done before it is applied on people. Although the research focuses on the needs of wounded soldiers, it could also find many uses in general medical care. For instance, emergency medical technicians could use it to treat patients with internal bleeding.





Leave your response!