First infant functionally cured of HIV
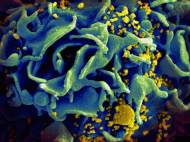 A group of researchers at the University of Massachusetts Medical School, the Johns Hopkins Children’s Center and the University of Mississippi Medical Center, recently revealed the first “functional cure” for Human Immunodeficiency Virus (HIV) in an HIV-infected infant. The finding represents a proof that infants can be cured of HIV and may help to eliminate HIV infection in children.
A group of researchers at the University of Massachusetts Medical School, the Johns Hopkins Children’s Center and the University of Mississippi Medical Center, recently revealed the first “functional cure” for Human Immunodeficiency Virus (HIV) in an HIV-infected infant. The finding represents a proof that infants can be cured of HIV and may help to eliminate HIV infection in children.
The HIV-infected mother had not received any prenatal HIV treatment, because she wasn’t diagnosed as HIV positive until just before delivery. A baby girl, born with HIV, received high doses of three antiretroviral drugs within 30 hours of birth. A series of test were done on the baby and they showed progressively reducing viral presence in her blood. Only 29 days after birth viral presence was undetectable. The infant received antiretroviral drugs for about 15 months, but then the doctor lost track of her mother and the baby didn’t receive adequate treatment. Ten months later, both standard blood tests and test for HIV-specific antibodies found no signs of active HIV.
According to researchers, prompt and intense antiviral treatment in newborns may help to remove the virus from their bloodstream before it could form so called hard-to-treat viral reservoirs – dormant cells that can swiftly re-infect a HIV patient once the treatment is stopped. Hence, by preventing these viral hideouts from forming, infants may achieve long-term remission without the need for lifelong treatment.
Previously mentioned baby girl is now considered as functionally cured, which means that the virus presence in the bloodstream is so small that lifelong treatment is not necessary and standard blood tests fail to detect HIV replication. Unlike a sterilizing cure, when all viral traces are entirely eradicated from the body, in functional cure condition the presence of viral traces is still noticeable by ultrasensitive methods.
“Complete viral eradication on a large scale is our long-term goal but, for now, remains out of reach, and our best chance may come from aggressive, timely and precisely targeted use of antiviral therapies in high-risk newborns as a way to achieve functional cure”, said Luzuriaga, M.D., PhD, UMass Medical School immunologist and professor.
Usually, newborns at high risk of HIV infection would get lower preventative doses of antiviral drugs for six weeks to prevent infection, and further therapy would continue if HIV is diagnosed half a year after the birth. However, the new case points up the potential for cure with early antiretroviral therapy and may change the current practice. The further study will show if this case is a highly unusual response to very early antiretroviral therapy or something that can be actually repeated in other high-risk newborns.
Experts say that natural viral suppression without treatment is very rare phenomenon and it usually occurs in less than half a percent of HIV-infected adults, so called elite controllers. Their immune systems are able to successfully suppress the virus to undetectable level for many years. Their ability has been greatly studied, and researchers are trying to find a way to help all HIV patients achieve the elite-controller status. The new case may be a turning point as it suggests that prompt antiretroviral therapy in newborns can help in achievement of a similar level of suppression.
Scientists claim that there is a single documented case of sterilizing cure so far. In 2007, an HIV-infected American living in Germany was battling both leukemia and HIV. When he underwent a bone marrow transplantation to cure his cancer, the surprise came when it cured both his cancer and HIV. Namely, the bone marrow came from a donor with a rare genetic mutation of the white blood cells which made the patient resistant to HIV. However, the procedure is dangerous and this treatment approach currently doesn’t represent the solution for 33 million HIV-infected people worldwide.
In spite of the fact that this case gives hope for infected newborns, the researchers claim that the main goal remains preventing mother-to-child transmission. It is estimated that antiretroviral treatments of mothers can prevent 98 percent of newborn infections, so it is important to emphasize that prevention is the best cure and hope for the newborns.
At this point, it is more likely that these findings will have more benefits for newborns than for adults. It is because the difference between the immune systems of babies and adults, as well as the places where viruses form their hideouts. Furthermore, in adults, it is much harder to pinpoint the time of infection. More studies are needed to be done and there are chances that possible solutions for adults may be discovered.





Leave your response!